Sometimes its hard to remember why I chose medicine as a career. It seems the idea of helping people, scientific discovery and lifelong learning were at the top of the list.
Nearly 25 years after starting as a pre-med I think those are still goals and in fact for the most part daily occurrences.
Initially, I thought about surgery. I probably had little idea what pathology was or did in the patient care continuum, or thought I knew beyond what I learned from Quincy, M.E..
My third week on the “wards” as a third-year medical student was spent on the cardiothoracic (CT) surgery service following 2-weeks of neurosurgery experience. Ruled out neurosurgery the first day following a 17-hour surgery on a patient who died in the hospital within a week of his surgery to remove a metastatic renal cell from his frontal and ethmoid sinuses and involving part of his frontal lobe in a combined neurosurgery-ENT case.
That experience however introduced me to the frozen section room and surgical pathology for the first time. The idea of looking at a small piece of tissue to determine diagnosis, confirm extent of resection or effect of prior treatment that would be used intraoperatively to help guide patient care seemed intriguing.
Two weeks later we admitted a middle-aged African-American female to the CT surgery service with 6 month history of shortness of breath, fevers, weight loss, night sweats and weight loss. Prior imaging studies showed significant mediastinal hilar adenopathy. The plan was to admit for lymph node biopsy via a transthoracic approach.
Bets were placed on what the diagnosis would be when the tissue came out. The fourth-year student, soon to be surgery intern and CT surgeon to be guessed lymphoma. Hodgkin’s Disease (Lymphoma) to be exact and predicted Reed-Sternberg type cells on the biopsy. The CT fellow predicted metastatic carcinoma from an unknown primary, or at least an primary other than lung since there were no lung masses and subsequently of little direct consequence to his practice which was limited to CT surgery. The surgical attending postulated starch intoxication. I was not sure what that was then and am less clear on what he meant now. It is hard to find any case reports or series documenting this clinical picture with “starch intoxication” as a possibility in the differential diagnosis.
I guessed sarcoidosis and predicted non-caseating granulomas on the biopsy.
Sarcoidosis is a poorly understood systemic inflammatory disease that can involve nearly every organ or organ system characterized by non-caseating granulomas and often a diagnosis of exclusion, as it is called, once other causes and possibilities for the granulomas are excluded. The differential diagnosis includes, among many other possibilities, lymphoma, metastatic disease, infections and apparently starch intoxication.
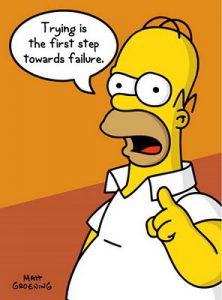 From the minute I opened my mouth and muttered “sarcoid” I was ridiculed about my choice among the differential. It was only appropriate. In medical training as with other forms of training and apprenticeship, stuff rolls downhill. The shorter your lab coat, the bigger your target.
From the minute I opened my mouth and muttered “sarcoid” I was ridiculed about my choice among the differential. It was only appropriate. In medical training as with other forms of training and apprenticeship, stuff rolls downhill. The shorter your lab coat, the bigger your target.
For a bunch of reasons I do not recall why, despite being admitted on a Monday as an inpatient, the patient was not taken to the OR until that Friday. Something about room scheduling, excluding tuberculosis before taking her to the OR and risk exposing others and the fellow’s schedule to do the procedure with the rooms CT had available to use that week.
The ridicule lasted the entire week. The fourth-year student, one-year to the day more experienced than I was perhaps the most incessant, if not humorous in his approach. No way was he going to buy me a beer over this one at the corner pub inhabited by med students for cheap beer and cheaper pool tables.
Friday came and our patient was taken to the OR. 6 months of clinical symptoms that we knew about, 1 week in isolation in a hospital room and time to drape, prep and anesthetize before a short 20-minute mediastinoscopy and biopsy.
Our team startled the pathologist sitting alone in the frozen section suite inside the OR. He wondered why 6 people had to bring in a single 2-centimeter piece of tissue having all broken scrub to carry it out of the room. He nearly tripped over his untied shoelaces before adjusting his thick glasses to see his peril. He stamped the specimen requisition and proceeded to nearly drop the specimen container upon getting it handed to him.
A few minutes later, with the help of a machine to rapidly freeze and cut a thin section to be stained and viewed under a microscope, the moment of truth was near. Who would be on the hook for a pitcher of Old Style?
The glass slide with the blue section of tissue clanked against the microscope stage. Focus on medium power and the pathologist remarked “What a beautiful sea of granulomas”. Not a Reed-Sternberg cell in sight. Later testing and exclusion of other etiologies through other stains for microorganisms and flow cytometry confirmed at least one person’s suspicion of sarcoidosis.
Pathology was ruled in and surgery was ruled out.
































