A simple and effective high-yield plan for digital pathology system validation
Here it is – a simple, easy to perform, highly reproducible plan for manufacturer pre-market approval or laboratory self-validation for the intended use of endoscopic mucosal gastrointestinal biopsies.
 These specimens are extremely common in nearly every hospital or community laboratory as well as the large commercial reference laboratories, specialty laboratories that focus their interests on gastrointestinal pathology & in-office laboratories that serve endoscopy practices.
These specimens are extremely common in nearly every hospital or community laboratory as well as the large commercial reference laboratories, specialty laboratories that focus their interests on gastrointestinal pathology & in-office laboratories that serve endoscopy practices.
According to a review from 2009, more than 55 million procedures were performed with GI endoscopic devices with nearly 50% of those colonoscopies. GI/endoscopy cases can make up 24% or more of cases performed in ambulatory surgical centers (ASCs). Gastroenterology is the most common specialty in both single- and multi-specialty ASCs. It is present in 34% of all ASCs and an average of over 3,700 GI procedures are performed annually in each ASC. Between 2000 and 2009, the percentage of ASCs offering gastroenterology procedures increased from 11% to 34%.
Endoscopic biopsies provide a finite amount of tissue derived from a number of organs: esophagus, stomach, duodenum, terminal ileum, colon and rectum. Routinely, particularly with upper gastrointestinal biopsies, Helicobacter pylori immunohistochemical stains or special stains (Diff-Quik) are performed on stomach biopsies as well as Alcian blue and/or PAS stains are performed on esophageal biopsies.
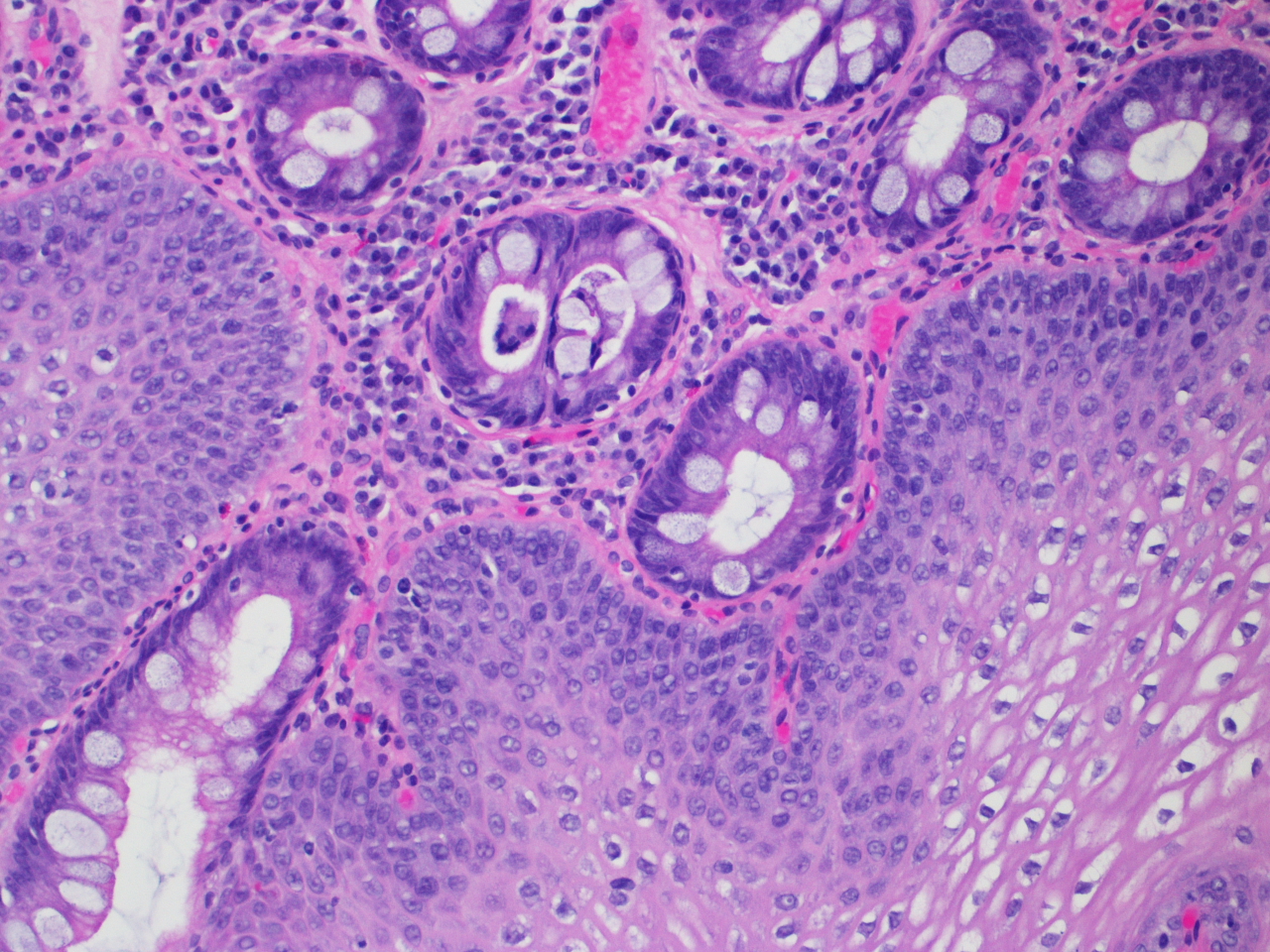 Terminology regarding classification of disease for the respective organs has become perhaps more standardized among laboratories than perhaps any other sub-specialty. For example, diagnoses such as “Specialized intestinal metaplasia consistent with Barrett’s esophagus; Negative for dysplasia” or “Moderately active chronic gastritis with numerous organisms identified morphologically consistent with Helicobacter pylori” are easily reproducible, limited in syntax across laboratories and widely used terms among pathologists with minor variations.
Terminology regarding classification of disease for the respective organs has become perhaps more standardized among laboratories than perhaps any other sub-specialty. For example, diagnoses such as “Specialized intestinal metaplasia consistent with Barrett’s esophagus; Negative for dysplasia” or “Moderately active chronic gastritis with numerous organisms identified morphologically consistent with Helicobacter pylori” are easily reproducible, limited in syntax across laboratories and widely used terms among pathologists with minor variations.
Thus, for a significant percentage of the volume a lab may produce, if not their total volume, one is able to efficiently process and scan 60 specimens from each organ with often times distinct clinicopathologic findings and standardized terminology for comparison of digital slides compared with glass slides with a sufficient “wash out” period as has been proposed.
Given the number of organs for potential biopsy and tissue acquisition, a set or several sets of 300 cases/accessions/parts or more with accompanying immunohistochemistry and/or special stains is easily attainable even in lower volume laboratories.
Moreover, questions related to the presence and/or degree of dysplasia in Barrett’s esophagus or severity of chronic changes in inflammatory bowel disease and reproducibility of diagnoses using whole slide compared with glass slide can be interrogated without the need for any special case selection as these are commonly asked clinical questions widely available routinely from gastroenterologists.
Comments (1)
william shipley, md


































That picture reminds me of the movie “Human Centipede”.