The Movat Pentachrome and Digital Pathology
My Director of Anatomic Pathology during the course of my residency was a Mexican-born pediatric and neuropathologist who spoke perfect Spanglish with a bunch of last names and some with hyphens. She was a great person and a great morphologist. Nearly every case had a decision reached on it between the gross, microscopic and clinicopathologic correlation with H&E stains alone. She did not train with and therefore did not use many special stains or immunohistochemical stains in her practice.
Electron microscopy would likely be done before either of those other modalities which she had a lot of experience with and relied upon for those rare cases that did not declare themselves to her on H&E alone and where a more significant magnification of cellular organelles and structures was needed.
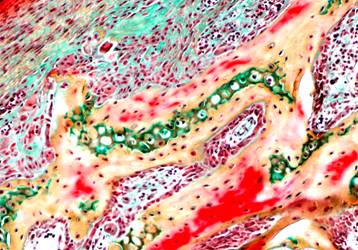 However, for really challenging cases, a Movat pentachrome would be used. This stain, as the name implies has 5 colors that stain different tissue types. Anytime she would ask you to order this the initial reply from the residents was “How will this help us?” and the response would be “It wont, but it takes the lab 2 days to do it and will give me time to think about the case, Senor.” After the first few times many of us learned to stop asking. Ultimately, she would make a decision relying on discussions with surgeons, radiologists, re-examining the gross specimen and the H&E dyed stains. The pentachrome stain justified the case as “non-routine” to track and measure the turn around times and exclude such cases to meet the % goal for a 2-day turn around time.
However, for really challenging cases, a Movat pentachrome would be used. This stain, as the name implies has 5 colors that stain different tissue types. Anytime she would ask you to order this the initial reply from the residents was “How will this help us?” and the response would be “It wont, but it takes the lab 2 days to do it and will give me time to think about the case, Senor.” After the first few times many of us learned to stop asking. Ultimately, she would make a decision relying on discussions with surgeons, radiologists, re-examining the gross specimen and the H&E dyed stains. The pentachrome stain justified the case as “non-routine” to track and measure the turn around times and exclude such cases to meet the % goal for a 2-day turn around time.
Even if immunohistochemical stains were available (and they were) to help differentiate particular lesions, she didn’t use them simply because she didn’t train on them so she didn’t use them. During the mid-90s this was probably “the norm” for pathologists in their mid-50s and beyond, and as a result, we as residents did not really learn immunohistochemistry until we had more junior attendings and learning it ourseleves in our early practices.
This was 20 years ago and the point is that the same can now be said of digital pathology. If you didn’t train on it, you may not have it in your practice. Or molecular pathology. Or electron microscopy now. It is like a language, if you don’t use it, you lose it. If you never learned it, it is hard to teach an experienced pathologist a new technology, to paraphrase a popular expression about dogs and tricks.
Fortunately, we have another generation of pathologists since those days who don’t remember life without whole slide imaging, image analysis algorithms, smartphones, iPads, cloud computing, social media and the Cubs finishing last every year.
Many medical students today, with what little histology they learn in medical school today, do so “virtually” or with “virtual slides” – not a good term – as if they are not “real” but they don’t have to rent a microscope and slide box and walk uphill both ways barefoot in the snow without a jacket anymore. Many pathology residencies have whole slide case conferences and scanning technology and image analysis being performed.
At the expense of electron microscopy, these medical students and residents will learn immunohistochemistry and molecular pathology and digital pathology and will understand what they need to arrive at the right decision for cases that come across their desk. And may never learn how to interpret a Movat pentachrome.

































