To Sign Out or Not to Sign Out? Part 2: The Fax Machine
 I received a lot of feedback offline about Part 1 of this post (see: “To Sign Out or Not to Sign Out? Part 1” ) from a number of pathologists echoing my sentiments on the issue of turnaround time in general and needs/expectations from clinicians and patients about getting their results in a timely manner. The consensus was little would be lost “holding” signing out cases – whether reviewing them and not signing them out or simply not reviewing them until after the holiday. Uncle Joe’s prostate cancer diagnosis or Aunt Sue’s breast cancer diagnosis might consume Thanksgiving dinner or Christmas or New Year’s celebrations. On the other hand, folks might be surrounded by friends and family to have discussions and make plans heading into a course of treatment decisions that will have to be made. It seems most of us, as we do any other day of the week or year, sign out the cases, call back new malignant diagnoses and expect another pile of slides the following day after the holiday to repeat the process. It is not so much a matter of turnaround time as it is keeping up with the workload and knowing tomorrow there will be more cases to result and reassure patients their biopsy is negative or confirm the suspicion they have a malignancy.
I received a lot of feedback offline about Part 1 of this post (see: “To Sign Out or Not to Sign Out? Part 1” ) from a number of pathologists echoing my sentiments on the issue of turnaround time in general and needs/expectations from clinicians and patients about getting their results in a timely manner. The consensus was little would be lost “holding” signing out cases – whether reviewing them and not signing them out or simply not reviewing them until after the holiday. Uncle Joe’s prostate cancer diagnosis or Aunt Sue’s breast cancer diagnosis might consume Thanksgiving dinner or Christmas or New Year’s celebrations. On the other hand, folks might be surrounded by friends and family to have discussions and make plans heading into a course of treatment decisions that will have to be made. It seems most of us, as we do any other day of the week or year, sign out the cases, call back new malignant diagnoses and expect another pile of slides the following day after the holiday to repeat the process. It is not so much a matter of turnaround time as it is keeping up with the workload and knowing tomorrow there will be more cases to result and reassure patients their biopsy is negative or confirm the suspicion they have a malignancy.
One pathologist summed it up best:
“This is the exact reason turnaround time (TAT) and the metric of TAT is pretty much bogus. All TAT measures is the time from accessioning in the lab to the time the result is certified by the pathologist. It ONLY is a measure of lab performance and has little to do with patient quality in my opinion for reason being 1) the time from the procedure to the time the tissue was accessioned is completely variable 2) the time from certification until the time the clinician reads the result is variable and 3) the time from when the clinical reads the result to notify the patient is variable. 4) I can sign out a bunch of cases as “pending” to meet TAT and then add in the actual result later. Some results the patient just gets a card in the mail “your pap is normal, schedule annual physical in one year” or “your colonoscopy showed benign polyps, however they types of polyps have determined you will need your next colonoscopy in 5 years”…there isn’t even a person to person notification! So why is it I jump through hoops to turn around a diagnosis in 24 hours or less (to meet administrator metrics)….when the patient gets a card in the mail weeks later than when the case was actually certified???? This never made sense to me. I think we are measuring the wrong thing………and I think in the coming era of MACRA to show that patient quality was actually improved we need to change the meaning of TAT and notification of results. Maybe the EMR should tally the time from accessioning until the result was clicked on by the provider? Or maybe when the result is given to the patient the provider has to clear the result off “the list” and then that time is the final TAT…..I think those stats would be more telling……..And do we really even know what the patient’s want? (I know what I would want!) ….A “rushed” diagnosis so they can get on their cruise ship? Or a properly attended to case needing additional levels, stains, consult, and time to provide the highest quality and accuracy which may not be ready before the long weekend?”
This brings up one of the most important issues regarding turnaround time and need for speed and “timeliness of reporting” and the like and if when you sign out a case – those results are actually shared with a patient as fast as the specimen was processed and read and a report created. For the sake of argument, let’s say on “routine” dermatology or genitourinary or gynecology cases where there is a significant likelihood of ruling out melanoma, prostate cancer or endometrial hyperplasia and the cases are completed within 24 hours of accessioning – do providers notify patients of the same within 24 hours?
Probably not.
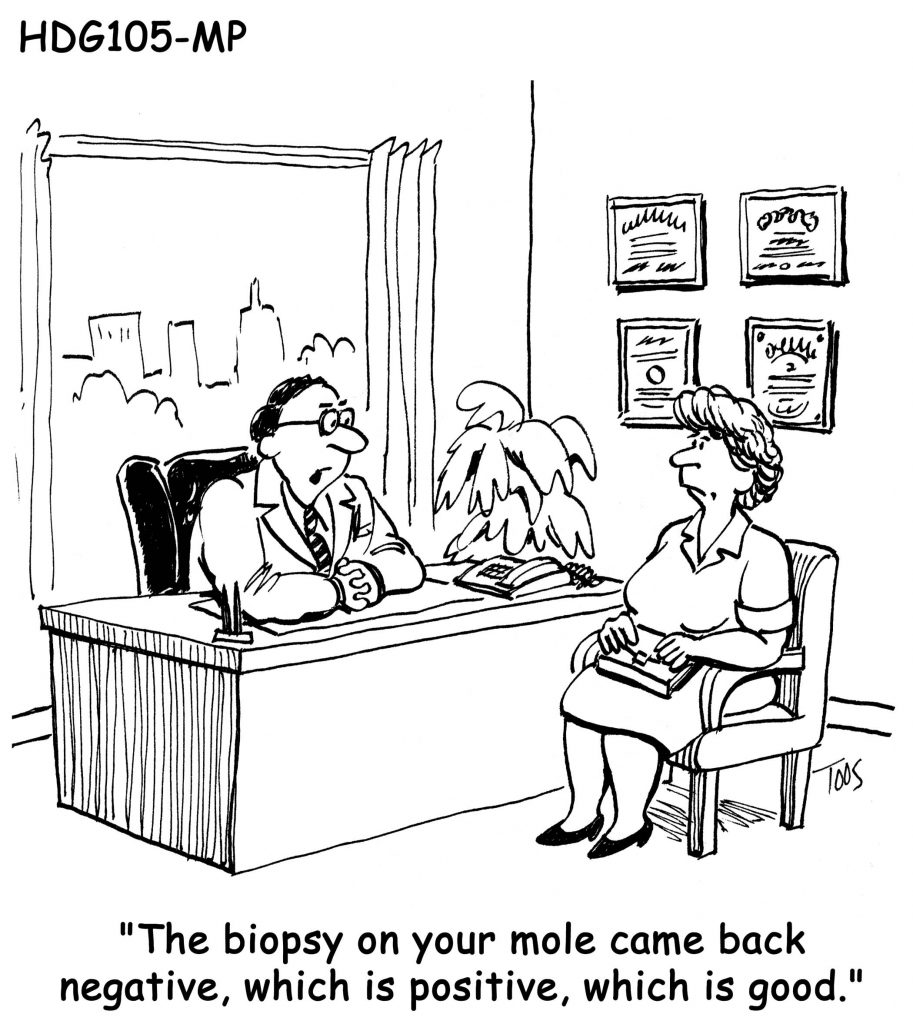
What does everyone hear when they get a biopsy? “We will get your results back from the lab in 2 to 3 weeks.” Been there, done that. Others have told me the same. They will call me in a couple of weeks. Meanwhile, the result may be in an electronic medical record (EMR) or on a fax machine.
This creates another layer. Results may be faxed to a provider’s office. And perhaps faxed to another provider’s office at the location where the patient was actually seen. And someone has to collect the faxes, look up the patients, put them in the appropriate mail slots or boxes for the appropriate “healthcare provider”, be it a nurse or physician assistant or physician to notify the patient or perhaps “release” the results in the EMR for patient’s to see in their portals. This is what may take additional days. The “certified result” by the pathologist may already be several days old confirming that pesky mole was a benign keratosis rather than a malignant melanoma. Or the 12 prostate needle core biopsies signed out in 18 hours show no evidence of malignancy.
But this is medicine. It may take weeks to see the provider, another period of time to schedule the biopsy, mammogram, colonoscopy or prostate biopsy. Then we complete our tasks within a day or two (including by the way the day after Thanksgiving, Christmas, New Years, Memorial Day, etc…) to send results to EMRs and fax machines to get reviewed perhaps days later.
As my pathology colleague summed up, it would be interesting to measure complete TAT from patient visit to biopsy to notification of biopsy result via post card, letter, phone call, EMR patient portal, etc… and think about how critical reading a biopsy inside of 48 hours of the specimen hitting the front door of the lab really is. After all, it seems “we will get your results back from the lab in 2 to 3 weeks” meets the consumer (patient) expectation, even if it is the holidays or a long weekend.

































