Different Sides of the Pond
 Great story in The Pathologist entitled “An Ocean Apart” — How pathology differs on either side of the Atlantic – and how it doesn’t by Michael Schubert
Great story in The Pathologist entitled “An Ocean Apart” — How pathology differs on either side of the Atlantic – and how it doesn’t by Michael Schubert
An outside look
How do other medical professionals view pathology? In this, at least, the countries see eye-to-eye. Rather than being determined by location, the respect pathologists are given by their colleagues seems to depend on how much day-to-day interaction the disciplines have.
“It’s variable,” says Michael Prystowsky, Chair of the Department of Pathology at New York’s Albert Einstein College of Medicine. “The working relationship between pathologists and oncologists, for example, is great. Everyone involved in cancer care understands what pathologists do, and we all work together very well.” But he cautions that other specialties, who have less contact with pathology, may not understand its role equally well. “Pathologists see themselves as professionals and experts in diagnostic medicine, and not all physicians appreciate that perspective. They may see diagnostic testing as a commodity – just order a test and deal with the results, and that can impact their professional interactions with pathologists.”
European pathologists agree. “I encounter many medical professionals who feel that pathology is very important for patient management,” says European Society of Pathology past President Han van Krieken. “But obviously, the ideas are mixed. It depends very much on the level and quality of interaction.”
Suzy Lishman, President of the United Kingdom’s Royal College of Pathologists, goes one step further and highlights one likely reason for the disparity. “We know that today’s new doctors qualify with less of an understanding of basic pathological principles than their predecessors,” she says, “particularly in universities where dedicated pathology teaching has been dropped from the curriculum. Not only does this mean that they are less able to understand what is happening to their patients, but also that they are less equipped to select appropriate pathology tests and to interpret the results when they receive them.”
The problem, it seems, begins early. A poor introduction to the discipline in medical school means that fewer students enter pathology – and also that those who choose other fields have a much less comprehensive understanding of who pathologists are and how they fit into patient care. “I don’t think trainees are exposed to pathology as much as they were in the past,” says Victor Tron, President of the Canadian Association of Pathologists. “There’s less pathology in medical curricula now, so we’re a bit mysterious to students. We’re trying to change that, but we’re fighting an uphill battle.”
“Most students enter medical school to diagnose and treat sick people,” says American Society for Clinical Pathology President William Schreiber. “The satisfaction, excitement, and human drama of dealing with living patients is hard to resist. By comparison, pathologists may seem introverted or antisocial, because our days are spent analyzing tissues and fluids from those patients. Many physicians move around the hospital during the day with an entourage of residents and students in their wake. Most pathologists spend the bulk of their time in labs or offices, available for consultation but not out on the front lines – and the difference in visibility makes an impression on students.”
Prystowsky sees an opportunity to make a difference. “As medical school curricula are changing, it’s important for pathologists to get involved when it comes to our professional activities – after all, we are the experts in diagnostic medicine.” And this is one thing van Krieken perceives as a distinct strength of European pathology.
Conversations with clinicians
Van Krieken, who is very familiar with US pathology practice, explains, “Large pathology departments interact with many hospitals, mainly through reporting. There is very little interaction by phone or face-to-face, because of distance or a lack of time.” He points out that, in difficult cases, it’s vital for the entire multidisciplinary team (MDT) – including the pathologist – to discuss the available options. “You can’t expect everyone on the team to know everything. It’s too much for one person. A team works best when each member performs their own specialized role and communicates well with the others.”
He offers an example from his own experience. “I received what I was told was a biopsy from a patient’s neck metastasis. It looked like adenocarcinoma with no special features, so I performed immunohistochemical staining to track down the primary tumor. I found prostate-specific antigen (PSA) positivity, so I reported that it was most likely metastatic prostate cancer, and the patient was given hormone therapy.
“But at the MDT meeting a week later, they showed more images and I realized that the tumor was actually extending from the floor of the mouth, rather than a lymph node in the neck. Perhaps it wasn’t really a metastasis at all. After studying a series of cases, I discovered that there is a special type of primary salivary gland tumor that exhibits PSA positivity – something we had never previously known. The patient didn’t have metastatic disease after all, but the primary tumor responded to hormone therapy anyway – and that’s now the standard treatment. Sometimes, you can only discover these things through the information that’s brought together in MDT meetings!”
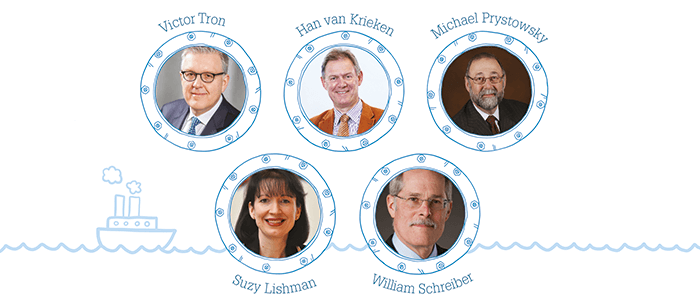
And North America is eager to learn. Prystowsky says, “I see the pathologist as an integral member of the healthcare team (see Figure 1). They’re actively engaged, providing diagnostic medicine expertise – which tests to use, how to perform them efficiently, how to explain the results to patients and care providers, and how to reach the right diagnosis in a timely manner and decide on the appropriate treatment.
“We need to focus on the pre- and post-analytical components by assisting our clinical colleagues on diagnostic ordering and interpretation,” agrees Tron. “Those two bookends are going to become increasingly important – and we can’t do that alone; we have to work with clinicians. They’re the ones out there treating patients, so we have to make them a part of this venture.” Tron’s workplace, St. Michael’s Hospital in Toronto, Canada, holds workshops to discuss bridging the communication gap between pathologists and treating clinicians, with the aim of understanding each other’s needs and frustrations – and generating ideas. Perhaps there’s a leaf to be taken out of the European pathology book…
Patients and the public
Although interaction with clinicians may vary widely depending on which side of the Atlantic you practice on, both sides agree that communication with patients and the public needs to improve. “My goal is to see pathologists talking more to patients,” says Schreiber. “There are opportunities to discuss what we do, explain diagnoses, and provide our medical opinions to the patients we serve. It’s the best way to demystify the profession and raise our public profile.” And demystification is certainly needed. “Whenever someone asks me what I do for a living, I say that I’m a doctor,” he shares. “They ask my specialty. After saying that I’m a pathologist, I allow a few seconds for them to respond, gurgle, or otherwise react. ‘That’s dead people, right?’ is a typical comeback.”
“I don’t think the public largely knows what pathologists do,” concurs Prystowsky. “It’s our responsibility to get out from behind the microscope, get out of the laboratory, and solidify our place as part of the healthcare team.”
On the other side of the ocean, the aim is the same. “One of the Royal College’s priorities is to highlight the central role that pathology plays in healthcare,” says Lishman. “Thousands of events have been held over the last few years to increase public understanding. There is still some way to go to dispel the myths, but I hope that high-profile pathology role models will help portray a more realistic and engaging side of the specialty.”
Lishman’s mission for many years has been to engage non-pathologists of all stripes, hoping not only to improve public awareness, but also to ensure that the best and brightest young students see pathology for what it is: a fascinating specialty worthy of their time and attention.
“We possess unique skills that other physicians need and, in most cases, they appreciate our expertise in helping them to diagnose and manage their patients. Without a pathology department, hospitals simply could not function. Both administrators and medical staff know this!” – William Schreiber
“Pathology must be recognized as a vital part of almost all patient pathways and worthy of investment, not seen as a back-office function and an easy target for cuts.” – Suzy Lishman
“It is important that we are recognized by our clinician colleagues, and that they see that we need resources to achieve results.” – Han van Krieken
“I’ve tried to focus on improving not just the public’s, but also medical students’ and trainees’ perception of pathology. We’ve tried to develop some leadership amongst our junior people, and we’re working on the best way to transition in the next phase of leaders.” – Victor Tron
The numbers game
Unfortunately, all of the engagement in the world won’t help if the discipline can’t solve one critical problem – the shortage of pathologists worldwide. Although there are notable exceptions to this rule (for instance in the Netherlands, where there’s actually a surplus of trained laboratory medicine professionals), most pathologists agree that there are simply not enough of them to maintain standards of care. “There’s a pending shortage of pathologists,” says Schreiber, “as well as a current shortage of medical technologists.” He cites ASCP Vacancy Survey statistics that reveal increased vacancy rates in all specialties except cytology and cytogenetics, along with the US Bureau of Labor Statistics’ estimation that the need for lab services will grow as much as 16 percent over the next decade.
But can supply keep up with demand? “We’re in a retirement cliff for pathologists in the United States,” says Prystowsky. “We’re an aging population, and we haven’t increased the number of trainees, so we’re heading for a deficit in the number of pathologists.” Everyone agrees that more candidates need to be recruited – but that’s much easier said than done.
“When I talk to people around Canada, there’s always the sense that they’re understaffed and workloads are becoming more complex,” says Tron. “It’s an uphill battle trying to convince the people with the money that additional positions are needed.”
“We should embrace cross-disciplinary and cross-professional roles, particularly in relation to molecular pathology. As ‘guardians of the tissue,’ pathologists are ideally placed to coordinate testing and integration of results and provide advice to clinical teams.” – Suzy Lishman
“Pathologists used to be those people in the basements of hospitals who gave you results and whom you didn’t often see.” – Han van Krieken
“I think that we are the definitive opinions when it comes to cancer diagnosis. I always say that radiologists provide a differential diagnosis and we provide the diagnosis. It gives me a lot of comfort to think that we make such a great impact.” – Victor Tron
“The pathologist needs to be central in the diagnostic testing, helping the team to choose the right tests and give the right analyses for each patient – but also to do study cohorts of patients longitudinally to improve treatment.” – Michael Prystowsky
The outlook for most of Europe is little better. “A recent report by Cancer Research UK described pathology services as being ‘at tipping point,’” says Lishman. “Many services are overstretched and understaffed at a time when demand is increasing. We know that many pathologists plan to retire over the next few years and in some disciplines there are too few trainees coming through to replace them.” Not only that, but many trainees opt for part-time work or shy away from smaller or less popular departments because so many are being closed or consolidated.
Some areas of Europe have an additional obstacle to overcome: the lack of available funding even when there are enough pathologists. Van Krieken highlights differences in the way pathology is perceived – and resourced – in different countries: “In Poland and the Czech Republic, there are very good molecular laboratories. But in places like Greece, Spain, Portugal or much of Eastern Europe, pathologists are often quite low-paid and low-ranked. So although they excel in areas like classical morphology, it can be very difficult to get access to new equipment and technology; they simply don’t have the resources.”
With shortages like this, though, come creative solutions. “In anatomic pathology, increasing workloads may require the help of technologists trained to screen tissue specimens,” suggests Schreiber. It’s a model that already works well in cytopathology and is ripe for expansion. He also proposes the use of telepathology to cover areas that lack local pathologists. Both solutions are ones that are gaining popularity in Europe as well.
“With increasing volume and complexity of work and a diminishing number of medically qualified pathologists, I believe that the roles of biomedical and clinical scientists will be further extended in coming years,” says Lishman. “The Royal College, working with the Institute of Biomedical Science, has recently developed a training program for biomedical scientists to learn how to dissect and report a limited number of surgical specimens. The first few scientists are nearing the end of their training and will soon be reporting cases independently. I hope that, as they start contributing to their department’s workload, they will be accepted and supported by their medical colleagues.”
No matter where one practices, it seems that pathologists are increasingly facing the challenges of limited staffing and resource availability. But as digital pathology gains followers, the world is shrinking – so it’s possible that pathologists on either side of the Atlantic Ocean will soon be able to turn to one another for help in surmounting those challenges.
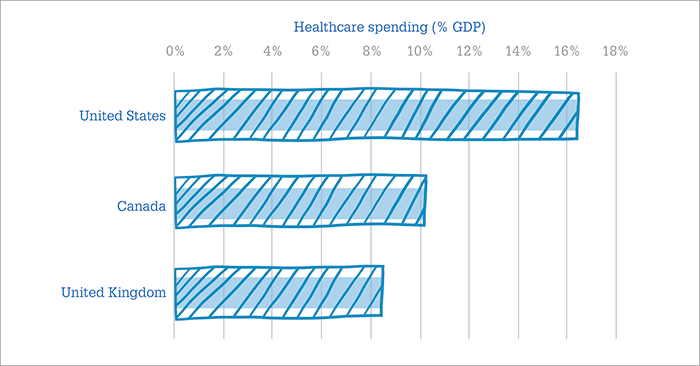
Hey, big spender
Speaking of difficulties specific to the United States and Canada, Schreiber says, “One major challenge is the sustainability of the two countries’ healthcare systems (see Figure 2).” Why such a great disparity in healthcare spending? “The introduction of new technologies – some of unproven value – is driving a portion of these costs. In the future, it will be necessary to justify the use of newer and more expensive tests. The American Board of Internal Medicine (ABIM) Foundation’s Choosing Wisely campaign identifies practices considered to be wasteful and unnecessary; to date, ASCP’s participation has resulted in 15 recommendations that, if followed, will reduce the cost of laboratory services.”
But how are these services funded in the first place? This is possibly the area of greatest difference from one country to the next – and, even now, it’s in flux. “The changes in the payment model are a challenge facing all of US medicine,” says Prystowsky. “We don’t know how that’s going to impact us. That’s why the pathologist has to be seen as an integral professional member of the healthcare team to improve time to diagnosis and enable implementation of an optimal treatment plan.”
Schreiber agrees. “At the level of public policy, pathologists need to demonstrate their involvement in promoting good patient outcomes. Reimbursement from governmental sources in the US will be increasingly tied to evidence of quality indicators. Because our services are part of a larger picture, it can be difficult to show how our practice directly affects patients – but we may be required to do so.”
Canada has the added complication that each province administers its own healthcare system. “The federal government really provides some general direction, but provinces run things day-to-day,” explains Tron. “Trying to coordinate things across the country also raises unique challenges. CAP-ACP tries to advocate for resources, but no two provinces have the same needs.” Although he’d like to see the country more united, he says it’s difficult to encourage the provincial governments to relinquish control. “I don’t think we are achieving the goal of having appropriate numbers of pathologists doing the work. I wish it were a bit more coordinated.”
Even in countries under a unified healthcare system, limited funding still poses a problem. “Most pathologists in the United Kingdom work within the National Health Service (NHS),” says Lishman. “Resources in the NHS are limited and the government’s priority is to maximize the efficiency of pathology services. Unfortunately, pathology is often seen as a ‘back-office’ function rather than an integral part of clinical pathways. One of my challenges is to persuade policymakers that investment in pathology can save far more money elsewhere along the patient pathway – by making timely diagnoses, detecting disease earlier, or even preventing it from developing at all.” Is there anything pathologists can do to help? “I suspect we’re in for tough times and further cuts before the value of investing in pathology services is recognized. It’s becoming increasingly difficult for pathologists to take time away from service delivery to contribute to national work – so if policymakers want expert input, they will have to consider how experienced pathologists can be released from other commitments,” she adds.
“Patients who have spoken with a pathologist involved in their care are usually quite grateful. They say that the pathologist took time to explain their diagnosis and may have saved their life. Direct patient contact makes a big difference in how our profession is perceived, and it’s an area where we can do better.” – William Schreiber
“The general public is basically unaware of what pathologists do, unless they have had to interact with one because they have a disease that needs to be explained. But once people have had that kind of experience, they become great advocates of pathology.” – Michael Prystowsky
“Many laypeople don’t have a good idea of what pathologists do. But in the end, for me, it’s not important to be recognized by the laypeople. As long as they get good diagnoses through the clinicians, I am fine with that.” – Han van Krieken
An imperfect split
For North Americans, the fragmentation of pathology also makes advancement and advocacy difficult. “Pathologists represent only two percent of all doctors in the US and Canadian systems, yet there are more than 30 organizations focused on pathology and laboratory medicine. The profession needs a collective voice to speak on policy and practice issues to government, our medical colleagues, and the public,” warns Schreiber. “Otherwise, we risk diluting ourselves until none of our voices are heard.”
Van Krieken has recognized the same phenomenon and sees integration as one of Europe’s strengths. “Very early on, we adopted molecular pathology as an integral part of pathology – and programs throughout Europe are pretty good. In the United States, they have the Association of Molecular Pathology, which is separate from the United States and Canadian Academy of Pathology. They work together, but they have separate meetings. I’m a strong believer in combining the two – so for me, that’s already a sign that the interaction is not optimal.”
In terms of training, though, the reverse may be true. Prystowsky emphasizes a significant difference in how pathologists are educated in North America and elsewhere. “Pathology has two major disciplines: anatomic pathology and clinical pathology (or laboratory medicine). In the United States, most of our pathologists are trained to do both; we view pathology as diagnostic medicine and both aspects are integrated.” He points out that in hematopathology, for instance, it’s vitally important to be able to make a morphologic diagnosis, use laboratory techniques, and apply molecular tests – all three are necessary for a comprehensive diagnosis and treatment plan. “That’s where we think pathology should be for all areas of diagnostic medicine. In Europe, there appears to be more of a split between training in anatomic pathology and laboratory medicine.”
In Canada, training is even more diversified. “Clinical pathology is broken into three distinct disciplines – hematopathology, medical microbiology, and medical biochemistry,” says Schreiber. “These clinical subspecialists tend to practice in large hospitals or private laboratories, where there is a need for full-time expertise in each area.”
Learning Lessons
Whichever training method one adopts, Europe – which has so much to teach North America about integrating pathology into diagnostics – knows it has a lot to learn about pathology education. “I think what we can learn from the United States is their rigorous education tools,” van Krieken says enthusiastically. “They are much more advanced than ours.” And with the rapid adoption of digital pathology, the transition to computer-based examinations, and even the use of simulations and virtual reality in teaching and training, it’s certainly true that North American institutions are moving ahead by leaps and bounds in the way that they educate the next generation of pathologists.
The next challenge? Pathologists from both continents agree that, with ever-increasing amounts of information to be crammed into a single residency, both curricula and teaching methods will need to change, if young pathologists are to keep up with their chosen discipline.
So is it true that North America and Europe are “two continents divided by a common practice?” In some ways, certainly – but in others, not so much. Despite differences in training, funding and even professional respect, pathologists around the globe are united by increasing workloads, staffing shortages, and the slow but steady shift from a traditional to a digital world. Most of all, though, what connects all pathologists is the same desire that drives any doctor: the goal to see every patient diagnosed, treated, and cured. And in that respect, it pays to reach out – because North American and European laboratory medicine professionals still have a lot to learn from one another.
Suzy Lishman is President of the Royal College of Pathologists. She is Head of the Department of Cellular Pathology at Peterborough City Hospital, Peterborough, UK.
Michael Prystowsky is Professor and University Chairman of Pathology at Montefiore Medical Center and Albert Einstein College of Medicine, New York, USA. He is a board member for the College of American Pathologists and Councilor for the Association of Pathology Chairs.
William Schreiber is President of the American Society for Clinical Pathology, consultant pathologist at Vancouver General Hospital, and Professor in the Department of Pathology and Laboratory Medicine at the University of British Columbia, Vancouver, Canada.
Victor Tron is President of the Canadian Association of Pathologists, as well as Chief of the Department of Laboratory Medicine at St. Michael’s Hospital, Toronto, Canada.
Han van Krieken is past President of the European Society of Pathology, Rector Magnificus of Radboud University, and past Chair of Pathology at Radboud University Medical Center, Nijmegen, Netherlands.