This is a piece I wrote for The Journal of the American Medical Association (JAMA) “A Piece of My Mind” section I actually hand delivered to the AMA building downtown on my bike from Northwestern that was probably rejected about as soon as it was filed for review as many of my short stories were at the time before I had my own way to publish what I wanted.
I had just finished my sophomore pathology final examination and remembered thinking about a question which involved testing your general knowledge about pancreatic carcinoma.
 This was a topic which I felt I knew about, having read the section in Robbins Pathologic Basis of Disease and reading the lecture notes several times before the exam. It was a topic I enjoyed reading and listening about since the instructor seemed genuinely interested in teaching the material and expected us to learn as much about the subject so that if we saw a patient with this disease we would be able to diagnose and treat the patient appropriately.
This was a topic which I felt I knew about, having read the section in Robbins Pathologic Basis of Disease and reading the lecture notes several times before the exam. It was a topic I enjoyed reading and listening about since the instructor seemed genuinely interested in teaching the material and expected us to learn as much about the subject so that if we saw a patient with this disease we would be able to diagnose and treat the patient appropriately.
The test question involved recalling that somewhere between 15 and 20% of pancreatic carcinomas arise in the body of the pancreas while another 5% arise in the tail. These figures are important because these tumors may grow silently for long periods of time and manifest themselves clinically only by extension to adjacent structures and metastatic spread.
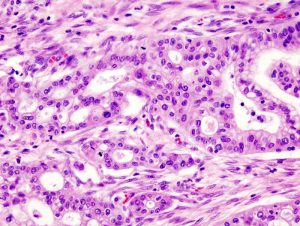
 For the remaining 60% of pancreatic carcinomas that arise in the head of the pancreas, obstructive jaundice may occur sooner while the tumor is smaller and before widespread metastasis has occurred. This is because these tumors are in a unique position to impinge upon the common bile duct, ampulla of Vater, or duodenum early in their life and present earlier.
For the remaining 60% of pancreatic carcinomas that arise in the head of the pancreas, obstructive jaundice may occur sooner while the tumor is smaller and before widespread metastasis has occurred. This is because these tumors are in a unique position to impinge upon the common bile duct, ampulla of Vater, or duodenum early in their life and present earlier.
As I was thinking about the exam and this question in particular the phone rang and startled me from my thought. The caller happened to be my grandmother who wanted to talk with me about some medical problems she had been having recently.
 She stated that for the past few days her skin had begun to itch all over and that she had an “odd taste in her mouth” for the past several weeks. She also stated that despite trying to eat as much as she could tolerate with this sour taste in her mouth she lost about ten pounds. In addition to the above complaints she mentioned that she noticed her skin “was not as red as it normally was.” And her eyes were yellow. This was especially worrisome for me since I knew my grandmother well, all of her past medical problems, her medications, allergies and previous surgeries.
She stated that for the past few days her skin had begun to itch all over and that she had an “odd taste in her mouth” for the past several weeks. She also stated that despite trying to eat as much as she could tolerate with this sour taste in her mouth she lost about ten pounds. In addition to the above complaints she mentioned that she noticed her skin “was not as red as it normally was.” And her eyes were yellow. This was especially worrisome for me since I knew my grandmother well, all of her past medical problems, her medications, allergies and previous surgeries.
These complaints were unlike any of her past medical complaints which most of the time were vague. Her past physicians ascribed these to “chronic fatigue syndrome”. When she called me with these new complaints she thought they were due to dust mites or “bed bugs” and fervently began to vacuum her entire apartment and wash all her linens. I knew this had nothing to do with any mites or allergies. I suggested she call her physician and schedule an appointment to be seen.
She was seen later that week by her physician who has been treating her for several years. He suggested she put some hydrocortisone cream on her skin to decrease the itching and call him in one week if it didn’t resolve.
As much as I didn’t want to believe it, I had an idea what this was and I knew that skin cream wasn’t going to cure what ailed her. But how could this be? She had no smoking history. She watched every calorie that she ate and had a well-balanced diet. She never worked as a chemist and wasn’t exposed to industrial agents. She was white, not black, and female, not male, and not a diabetic.
As I tried to recall all the risk factors that I memorized the night before I thought to myself she didn’t have any of the classic risk factors. How could this be? I tried to think of what could cause her to be jaundiced. Possibly it was primary biliary cirrhosis, or a gallstone, or maybe even a Klatskin tumor. A mass in the duodeunum was an even less likely cause.
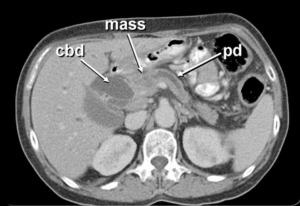
I told her to see her physician again and ask to have an ultrasound of the abdomen and liver function tests performed. The ultrasound confirmed a mass in the head of the pancreas with a dilated bile duct measuring 17mm in diameter. Her alkaline phosphatase and total bilirubin were through the roof. Still, she denied abdominal pain, back pain, nausea, or vomiting. She had no history of recurrent pancreatitis or migratory thrombophlebitis.
The radiologist had her admitted immediately for decompression and evaluation of this mass. The admitting diagnosis on the chart was pancreatic carcinoma.
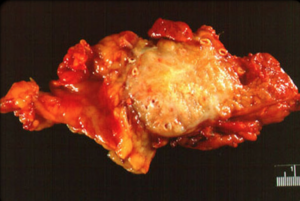
Once the work up was complete a general surgeon was consulted. She underwent a 10-hour Whipple procedure and pulled through it beautifully. The final pathology report described the mass as a well-differentiated adenocarcinoma with no nodal involvement. She subsequently underwent adjuvant radiation therapy and continues to be disease free.
That beautiful red color which disappeared from my grandmother’s face for a few days last winter has returned to its original glow. She just celebrated her 79th birthday and is spending this winter in Florida.
In medical school the often teach that early recognition of disease patterns and clinical signs and symptoms can make a difference. This is one case I will never forget.
My grandmother’s operation took place on the day/night that President Nixon passed away – having watched the coverage of it for hours in the surgical lounge. While she survived the Whipple procedure the quality of her life would never remain the same as before cancer and she was largely confined to her apartment relying on friends and family to help take care of her. Many trips on my bike or by cab in bad weather to her apartment a few blocks away from mine allowed me to watch firsthand the daily struggle with this dreaded disease.
She would live almost 2 years after her surgery, passing away on April 10th, 19 years ago today, at the end of Passover, as with this year, about six weeks before I finished medical school. She wanted to be there. Northwestern even offered to have a private ceremony in her apartment to see me getting “hooded” and have a diploma printed in time for her to see her grandson graduate from medical school. She kindly refused the offer, fighting to her last day to attend the ceremony. It wasn’t to be.
































