“Herceptoid” and “Personalized” Medicine
Over the summer a longtime friend asked if I could review some slides for a friend of his, or actually from his friend’s wife. Of course I agreed to do so. He mentioned that she had “metastatic breast cancer” and wanted to make sure the slides fit that diagnosis to insure she was getting the appropriate therapy. It seemed simple enough. The patient had been evaluated and was undergoing therapy at a well-known cancer center.
The patient initially presented with complaints of hip pain and was initially given paid medications and referral to physical therapy. Months passed and the pain continued. After an MRI revealed a large hip mass, a fine needle aspirate (FNA) and core biopsy were performed that demonstrated a metastatic adenocarcinoma. A battery of immunohistochemical stains later and the mass was felt to be “most consistent with breast primary”.
Subsequent imaging with CT of chest, abdomen and pelvis showed a lung mass, small compared to the hip mass. This also underwent FNA and core biopsy and showed an adenocarcinoma. After 2 sets of immunohistochemistries (IHCs), this too was felt to be “metastatic adenocarcinoma most consistent with breast primary”.
The patient had 2 reportedly normal mammograms and normal breast MRI exams.
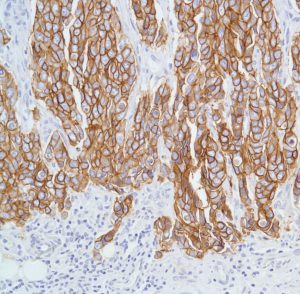 The slides I reviewed from the lung and hip showed an adenocarcinoma with the tumor cells strongly and diffusely positive for HER2 and negative for breast and lung specific markers (e.g. mammaglobulin, GCDFP-15, TTF-1, Napsin A and others).
The slides I reviewed from the lung and hip showed an adenocarcinoma with the tumor cells strongly and diffusely positive for HER2 and negative for breast and lung specific markers (e.g. mammaglobulin, GCDFP-15, TTF-1, Napsin A and others).
It didn’t quite fit together.
How did we get to metastatic breast cancer?
After discussion with the patient and his willingness to do so, I spoke with the patient’s oncologist. He was troubled by the matter as well. The patient was “HER2 positive” but the masses were not getting smaller on Herceptin and breast cancer chemotherapy, but rather she was having disease progression, particularly in the hip/pelvis.
Nonetheless, he mentioned she was “Herceptoid” and should be responding to Herceptin.
“Herceptoid” is probably the only word I have ever googled that did not come back with a single result.
Personalized medicine offers so many opportunities to provide targeted therapies to destroy tumor cells with less impact to cells in the patient. Many years ago a friend of mine shared a story about his father in-law’s oncologist who told him “John, if the cancer doesn’t kill you, the chemotherapy will”.
Those days are behind us for more and more cancers with oral-based regimens that are far less toxic with fewer side effects than conventional therapies of yesterday but has the pendulum swung too far?
Physicians use to treat patients. Then we began treating tumors. Now we are treating protein expression patterns or gene profiles or up-regulated/down-regulated genes or single mutations.
It is very exciting but what happened to treating the patient or at least the respective “abnormal growth” in conjunction with the other clinical findings, imaging studies and ancillary stains, including the negative imaging studies and stains that may make a tumor less likely rather than getting a hit for a particular gene amplication and a transmembrane protein subsequently increased that we can measure with light microscopic techniques?
Technically, the patient was not “HER2” positive although her tumor may have been, does not make the tumor breast cancer. We assign that because we have a drug for that which is not without its own risks but also with tremendous potential benefit.
If it quacks like a duck and looks like a duck, it is probably a duck but if it is HER2 positive does not a breast cancer make, particularly without a breast mass and other possibilities.
The patient subsequently underwent upper and lower endoscopy and a pelvic exam. Additional tissue from the hip/pelvis mass was sent to “a special lab in Michigan to find out what the tumor was” according to the patient’s family. No conclusive result was returned. Another oncologist suggested the possibility of an ovarian cancer metastatic to lung and bone that happened to be HER2 positive.
Are we personalizing medicine or de-personalizing it?
































