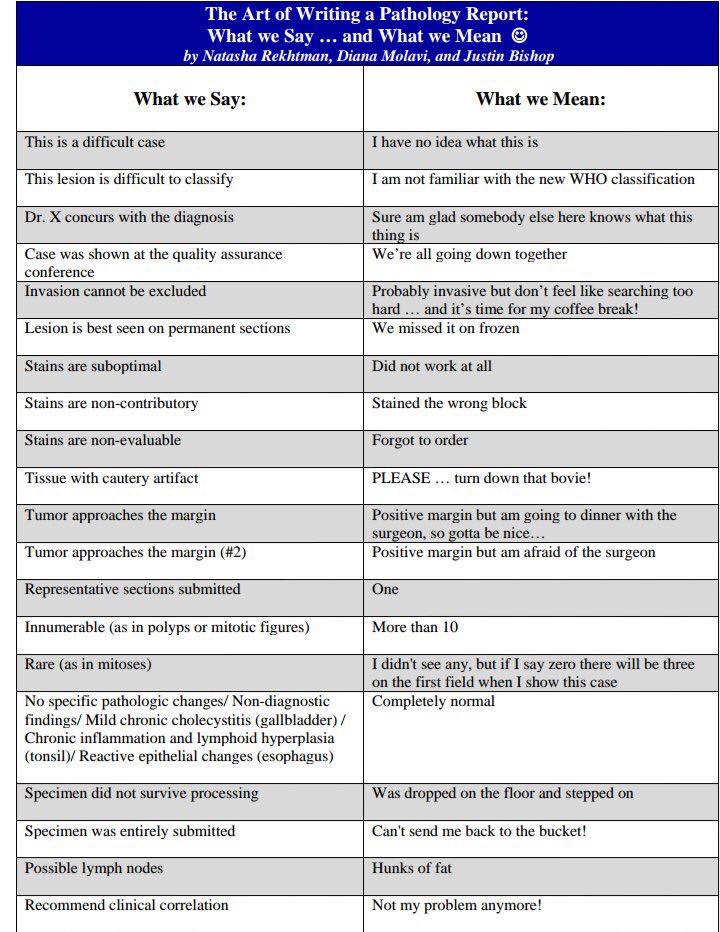
The Art of Writing a Pathology Report: What We Say and What We Mean
Over the weekend I shared an image on Facebook that garnered a lot of interest so I thought I would share it with readers here and add to the content. The image I believe comes from a book edited and largely authored by Natasha Rekhtman and Justin Bishop along with Diana Molavi in Quick Reference Handbook for Surgical Pathologists published by Springer in 2011.
Many years ago Dr. Philip LeBoit wrote an editorial in the American Journal of Dermatopathology with the title of “You Mean It, But Do You Say It?” based on another eidtorial from 1979 in the same journal with a similar title (Leider M. You say it, but do you mean it? [editorial]. Am J Dermatopathol 1979;1:223-4.).
His musings on what pathology reports say and what they mean are below the illustration below with his comments in italics with references to his subspecialty of dermatopathology.
We probably can all do a better job of saying what we mean and meaning what we say.
And who says pathologists don’t have a sense of humor?
Technical Factors
* “The specimen did not survive processing.” (It still exists somewhere, but the chances of finding it are slimmer than locating the body of Jimmy Hoffa, and those in the lab who know where it is are similarly loquacious to those who know the final resting place of Mr. Hoffa.)
* “The specimen is small and fragmented.” (Polymerase chain reaction studies might reveal human DNA, although 90kb segments were the longest that would be recoverable.)
* “Immunofluorescent studies could not be performed as the tissue was received in formalin.” (Despite dozens of phone calls and shipments of transport medium, the referring physician’s office will likely never successfully send us a specimen on which this test can be performed.)
The Microscopic Description
* “There is electrocautery artifact.” (If the dermatologist’s office were in a modern building, the smoke detectors would have gone off.)
* “Morphologic features are to some extent affected by crush artifact.” (Forces of over 2000 p.s.i. were applied in a twisting motion using a wrench, resulting in a section of lymphocytes that could have been hand painted by Jackson Pollack, if he had had paintbrushes of 2 micron width.)
* “There is only a very sparse, focal infiltrate of lymphocytes.” (There is no appreciable lymphocytic infiltrate, but you expect me to see something so I will say this to be “collegial”.)
* “Mitotic figures are rare.” (I did not see any, but am afraid that someone else might, and a lawyer might use the finding of a single mitosis to impugn my judgment.)
The Diagnosis
* “Histologically unremarkable skin.” (You may have missed the lesion completely after injecting anesthesia and biopsied uninvolved skin. Alternatively, you may have had a slow day at the office and felt the need to do something.)
* “Neoplasm of uncertain biologic behavior.” (Please don’t do anything extreme to the patient, but don’t blame me if things turn out badly for them!)
* “Changes consistent with the patch stage of mycosis fungoides.” (I am trusting your clinical judgment a great deal. If you as a clinician did not think that the patient has mycosis fungoides, you erred by putting that diagnosis on the requisition slip, because I have taken up your suggestion. Similar specimens sometimes come from those who do not have the disease. And, by the way, are you planning to refer the patient to an oncologist? If so, we had better talk.)
* “Slight epidermal hyperplasia and hyperkeratosis.” (Basically, the biopsy procedure was inadequate. You should either sharpen your curette or try anabolic steroids to develop the heroic strength that it takes to penetrate the granular layer across a broad front. By the way, the inference that the epidermis is hyperplastic is just a guess, as it is only represented by three keratinocytes.)
The Note
* “Conservative reexcision may be indicated.” (Barring the patient having only days to live because of another malady, you had better make sure that this thing comes out.)
* “Our experience is that lessons of this type behave in a benign fashion.” (To date, I have not been sent a subpoena in a matter regarding a case of this type. Of course, they may be saving these up for a class action suit.)
* “If this is a partial biopsy of a larger lesion, it may not be representative of the remainder of the lesion.” (I hope you are not so foolish as to think that a partial biopsy of a melanocytic lesion is similar to sticking a thermometer into a water bath. If I had more time, I would have tried harder to call you and find out how large the lesion was and what it looked like, and if you had more time you would have told me.)
* “Clinical follow-up information would be gratefully appreciated.” (I really, really would like to know, but I know that there is no CPT code for “transmission of follow-up information”, so my expectations that you will take the time to reply are limited.)
Comments (1)
Justin Bishop

































Glad you enjoyed the table! I was unaware of Dr. LeBoit’s similar musings, but they’re right on the money.
Justin Bishop, MD
Baltimore Maryland