“You see any escapees in there Doc?”
It was a Tuesday afternoon at Walter Reed Army Medical Center when I was called to see a patient in the Internal Medicine Clinic (IMC) for a fine needle aspiration (FNA) of a palpable neck mass. It was one of the days when Pathology ran a FNA clinic either in our department or with a cart with stains and a microscope we could bring to the patient. These services were becoming increasingly common in practices all over the country. For palpable masses, lumps and bumps that we could access without imaging, many of the clinical services sent their patients to us or called us to perform FNAs.
The patient we were scheduled to see, according to the primitive electronic medical record we could access, was a retired Marine Gunnery Sergeant with a history of a head and neck squamous cell carcinoma. He had prior surgery, chemotherapy and radiation and the clinical concern today in the clinic was a metastasis to a lymph node.
My medical student and I assembled the cart with the consent form on a clipboard, stains, clean water to rinse the stains, needles, syringes and the like and went down to the IMC. On the way I told/asked the medical student not to say a word while we were looking at the slide(s) in the room with the patient just a few feet away. While we could in most cases render a diagnosis, I usually left that to the primary clinician. Even years later, I realized I was still not well equipped to deal with delivering diagnoses in these situations and certainly wasn’t many years earlier (see: Christmas Eve FNA).
The patient stood up when we entered the room and greeted us a Second Lieutenant and Major, as the medical student and I entered the room. The Gunnery Sergeant mentioned he knew what we were there for and didn’t need it explained to him any further having been through the procedure before. I explained we still had to provide informed consent and would do so.
The patient was a veteran of the Vietnam War and after a career of more than 25 years as he explained to us, was looking forward to doing something else when he became ill years earlier. He had the injuries and battle scars of war as well as from the operations and radiation. His faded tattoos highlighted a life of military service and his travels all over the world multiple times. The Gunnery Sergeant joked around with the medical student about being in the Navy.
The needle went in and immediately there was a “grittiness” as the medical student ever so slightly pushed the needle back and forth beneath the skin “to collect cells to look at under the microscope” as the consent form had pre-populated. Usually benign lymph nodes and masses do not have the “grittiness” under the needle. The pre-test probability was high for a lymph node metastasis and the “gross examination” was starting to confirm that suspicion.
I took the needle from medical student and prepared the slides, some air-dried and others to be fixed in alcohol for staining and review the next day with other stains (rapid Diff-Quick versus Pap stain). The purple stained cells were obvious as I rinsed the slide. I handed the slide to the medical student and watched the images from the other set of objectives.
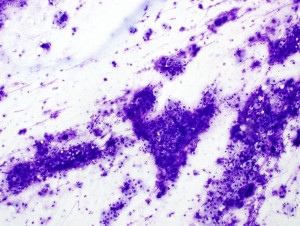 There were tumor cells everywhere that represented squamous cell carcinoma. We had enough material to render a diagnosis.
There were tumor cells everywhere that represented squamous cell carcinoma. We had enough material to render a diagnosis.
Just about then the Gunnery Sergeant asked, “You see any escapees in there Doc?”
I explained, as I did in these situations, that we would look at the other half of the slides tomorrow and call the treating physician. I thought I was in the clear.
But, despite my telling/asking my medical student to not say a word about the slides, did.
He asked, “What are all those big atypical looking cells in there?”
Casually, as I was unplugging the microscope from wall, I said “Those are macrophages” and pushed the medical student out of the room along with the cart and slides with malignancy on them. Further down the hall, I saw the patient’s oncology fellow who I knew from internship and let him know that the FNA was positive for malignancy.
What happened next between myself and the medical student I will not record here but for the next 3 weeks on his pathology rotation he never spoke during another FNA again.


































